HS is a chronic, recurrent, and debilitating inflammatory skin condition. While it can occur at any age, it usually presents after puberty. It is characterised by lesions on the skin, including abscesses, painful nodules, draining tracts and fibrotic scars.5,6 The exact underlying cause of HS is unknown. But it’s thought to be due to a combination of genetic, environmental and hormonal influences.7
The prevalence of HS in Europe is estimated to be 1% or more. This means there are currently over 7 million people living with HS in Europe alone.1,8 It affects three times as many women than men.3 Although HS is considered a common condition, it’s often misunderstood.
HS in the armpit across Hurley stages:
The Hurley staging system describes three clinical stages, and is commonly used to assess the severity of HS:5

Stage I
Single or multiple abscesses without tunnels or scarring.

Stage II
Recurrent abscesses, single or multiple widely separated lesions, with tunnels and scarring.

Stage III
Diffuse or broad involvement, with multiple interconnected tunnels and abscesses, and scarring.
Images reproduced from DermNet New Zealand. Distributed under the terms of a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 (New Zealand) License: https://creativecommons.org/licenses/by-nc-nd/3.0/nz/.9
HS pathogenesis9
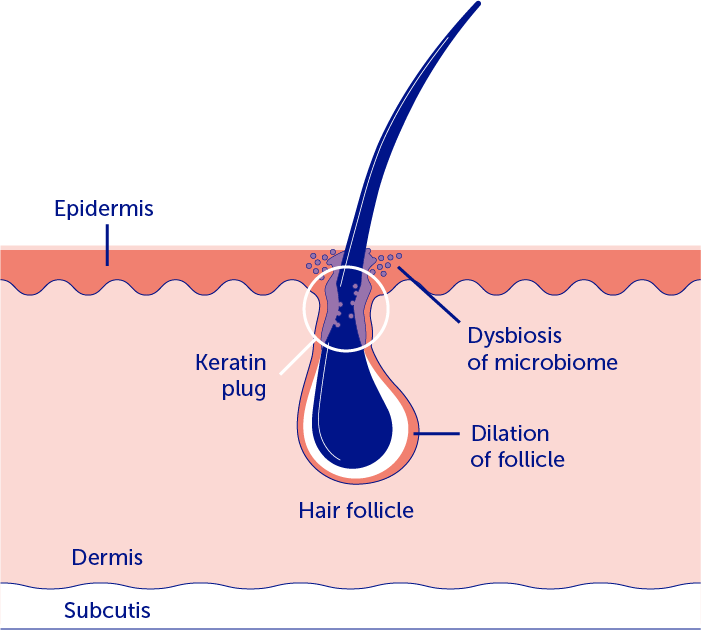
1. HS is initiated by follicular occlusion and dilation
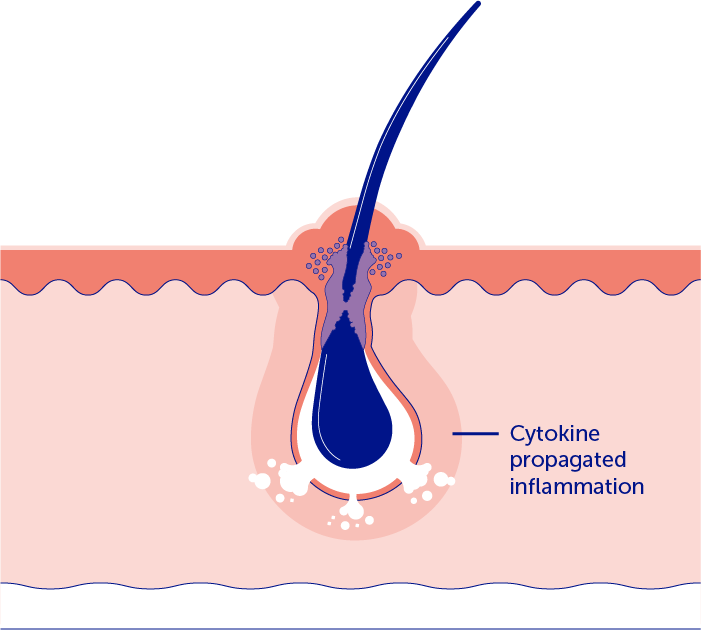
2. Subsequently, the inflammatory cascade with cytokine-driven positive feedback results in follicular rupture and the formation of inflammatory nodules and abscesses
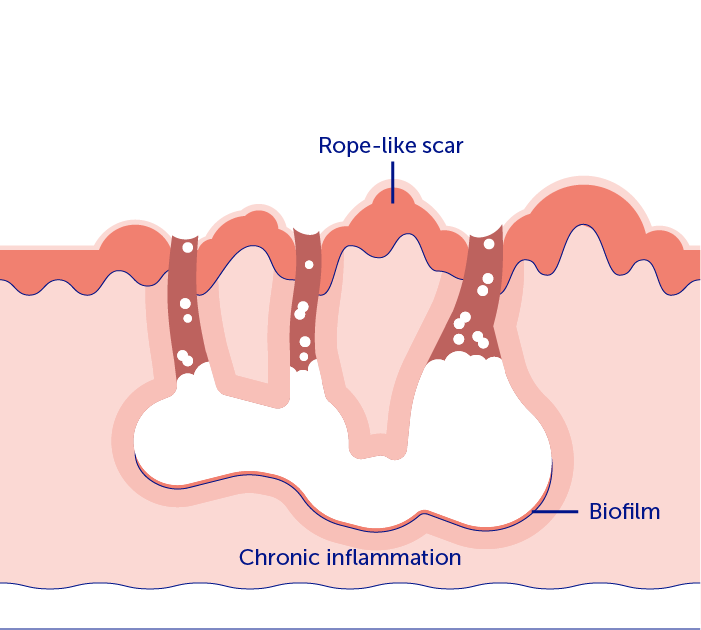
3. A chronic state of inflammation and imbalance of fibrotic factors eventually leads to tunnels and scar tissue
Image adapted from Goldburg SR, et al. J Am Acad Dermatol. 2020;82:1045–58.
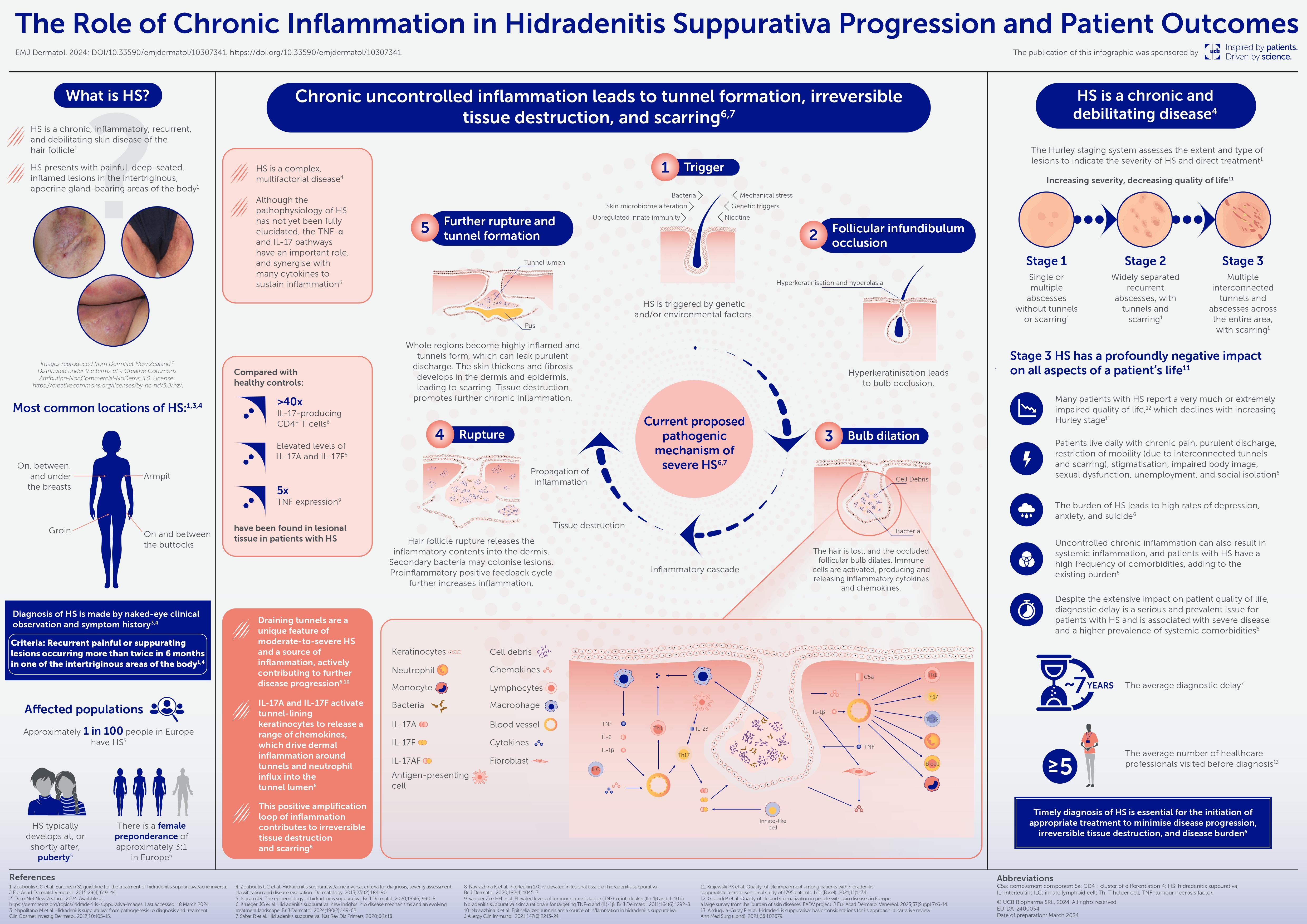
Learn more about the pathogenesis of HS and the importance of early diagnosis and treatment to prevent disease progression in this handy infographic
The need for change
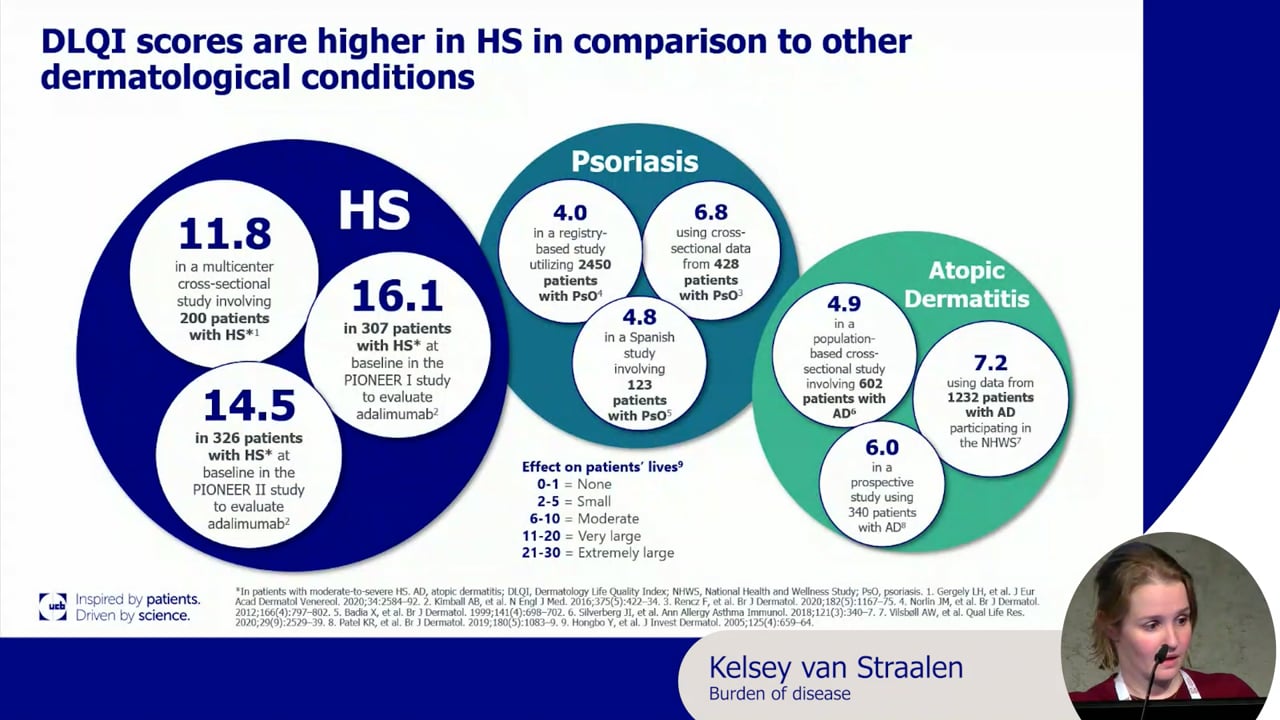
Many patients with HS live with unbearable pain, every day. The physical symptoms, fatigue, and high comorbidity burden, coupled with the isolating and stigmatising nature of the disease, dramatically affect quality of life.4,9
It’s no surprise that HS is ranked in the top five skin diseases with the most negative impact on patients’ quality of life.10
It’s time we raise awareness of this debilitating disease and help improve the lives of people living with HS.
Only through educating all those involved in the management of HS can we strive to shorten the time to diagnosis, alleviate the patient burden, and optimise the management of HS for our patients.
Find out more about our commitment to improving HS care

The burden of HS
Find out more about how we are raising awareness of HS to eliminate diagnostic delays
HIDRACENSUS 7.3 programme
Learn more about our ongoing
expert-led initiative, which aims to enhance the standard of care for patients living with HS across Europe

HS Learning Hub
From bench to bedside, follow the story of HS through our educational curriculum

Under the Skin
HS affects all aspects of a patient’s life. Listen to the latest episode of ‘Under the Skin’ here, and find out more about what you can do to alleviate this burden
References
- Ingram JR, et al. Br J Dermatol. 2020;183:990–8.
- Barmatz S, et al. Dermatology. 2022;238:772–84.
- Nguyen TV, et al. J Eur Acad Dermatol Venereol. 2021;35:50–61.
- Howells L, et al. Br J Dermatol. 2021;185:921–34.
- Zouboulis CC, et al. Dermatology. 2015;231:184–90.
- Anduquia-Garay F, et al. Ann Med Surg (Lond). 2021;68:102679.
- Diaz MJ, et al. Curr Issues Mol Biol. 2023;45:4400–15.
- Worldometer. Europe population. https://www.worldometers.info/world-population/europe-population/. Accessed June 2024.
- Goldburg SR, et al. J Am Acad Dermatol. 2020;82:1045–58.
- Tzellos T, Zouboulis CC. Exp Dermatol. 2022;31(Suppl 1):29–32.
EU-DA-2300369
Date of preparation: January 2024