
Female patients are particularly impacted by chronic rheumatic diseases, with a lower quality of life and a higher burden of disease.1–6 Women are increasingly choosing to start a family later in life; however, treatments to control rheumatic diseases are often started at a younger age.7
It is therefore critical that disease remission is achieved to prevent disease progression, maintain quality of life and aid optimal foetal outcomes.8–14 Despite this importance, many patients do not feel accurately informed about their treatment options during their childbearing years.7,15
Timely shared decision-making discussions enable women of childbearing age to make informed choices regarding treatment options, taking into account potential disease outcomes and future plans.7,16–19 Find out more about how you can address these unmet needs to help improve treatment outcomes for your female patients.

HEAR FROM THE EXPERTS
Achieving clinical remission for your female patients of childbearing age
with Prof. Andreoli
Achieving and maintaining clinical remission for women of reproductive age accommodates diverse reproductive goals and timelines.7
Prof. Laura Andreoli discusses the increased burden of disease for women of childbearing age with chronic rheumatic diseases, including the implications of not achieving clinical remission in these patients. Prof. Andreoli explores strategies to help these patients achieve clinical remission, highlighting the importance of proactive family planning discussions which can facilitate a treat-to-target treatment strategy.
“It's important to plan today for tomorrow, so it means that achieving remission as early as possible.”
Prof. Laura Andreoli
University of Brescia, Brescia, Italy
Knowing future plans of your female patients could improve their treatment outcomes
Understanding the future plans of female patients is important for improving treatment outcomes, especially as diagnosis and treatment for axSpA, RA and PsA tend to overlap with their reproductive years.7,16,19
However, there exists a notable gap in patient education, as many women report feeling inadequately informed about their treatment options.7,15 Engaging in timely discussions can inform patients about their treatment options and facilitate a shared decision-making process that aligns with their current health needs, as well as their future plans.7,16–19

HEAR FROM EXPERTS
The importance of future planning with female patients with chronic rheumatic diseases
with Dr Oseme Etomi
Watch the interview video below, as Dr Oseme Etomi examines the importance of discussing future plans with female patients who have chronic rheumatic diseases. In her answers, Dr Etomi:
- Elaborates on the key stages in the female patient journey where conversations regarding treatment management should take place
- Explains the importance of early dialogue to ensure patients have all the required, and accurate, information to help make an informed treatment decision
- Emphasises the importance of clinical data in helping guide these vital conversations and facilitate a shared decision-making process between the clinician and patient, ensuring patient choices are informed and compatible with future pregnancies
“It's really important for us to tell these patients the right information at the beginning and then checking at various time points within that treatment journey.”
Dr Oseme Etomi
Guy's and St Thomas' Hospital, London, United Kingdom


Bridging the information gap for your female patients
Women aged 18–45 with chronic rheumatic diseases often have limited information on how to best manage their condition throughout their lives.20
Early shared decision-making is crucial for women with chronic rheumatic diseases, including identifying the risks and benefits of treatment. By initially guiding informed choices, future interventions can be minimised. Without these conversations, women may potentially delay pregnancy, face treatment concerns or avoid treatment altogether during pregnancy.12,17,19,20


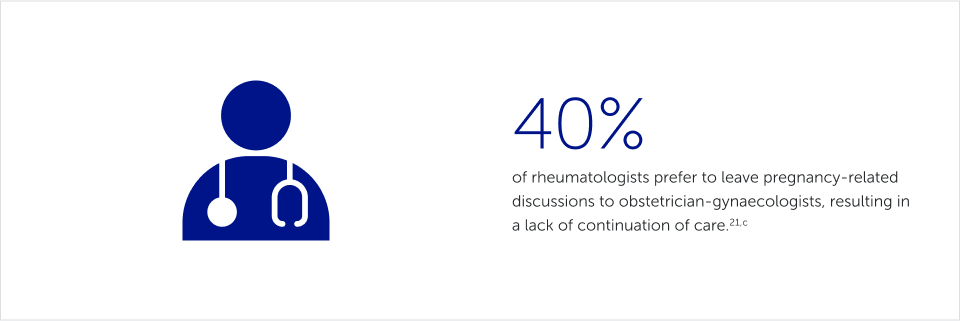

Greater awareness of family planning in disease management could improve shared decision-making conversations, ensuring a more integrated approach that better meets the needs and priorities of your female patients during their reproductive years.18,21,22
FREE E-LEARNING COURSE
Clinical communication strategies with GRAPPA to improve patient outcomes
Guidelines recommend shared decision-making across rheumatology, which is proven to improve patient satisfaction and adherence to treatment.9,17,22–24 Communicating with patients is key to the patient-clinician collaboration, yet this can be challenging in an increasingly complex treatment landscape.9,17,22–24
The Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA) have developed a skills-based e-learning course for healthcare professionals working in rheumatology to improve consultation skills.27
Gain valuable insights into effective clinical dialogue that can positively impact your daily practice. The 60-minute course delves into the importance of active listening, offers techniques to master clinical communication and presents a clinical case to apply these skills in practice.27 Hear from fellow healthcare professionals as they share their experiences and takeaways from the course.
This course was funded by an unrestricted education grant from UCB

GRAPPA course
The e-learning course is available to GRAPPA and non-GRAPPA members alike, so please share with your colleagues and others in patient care roles.

Other articles you might like
Recommended Articles
You can read more articles that might interest you.
Want to see more articles?
Can’t find the answer you’re looking for? See all the Resources we have.
EU-DA-2500046
Date of preparation: March 2025



