Learn about the causes and underlying pathophysiology that drive psoriasis, including the role of cytokines (TNF and IL-17/23) and intracellular signalling. Discover how a self-amplifying cycle involving IL-17 drives inflammation in psoriasis.

Date of preparation: December 2024
Learn about the causes and underlying pathophysiology that drive psoriasis, including the role of cytokines (TNF and IL-17/23) and intracellular signalling. Discover how a self-amplifying cycle involving IL-17 drives inflammation in psoriasis.
Causes & pathophysiology of psoriasis
Psoriasis is mainly studied as an autoimmune condition, and it is now well established that psoriasis is the result of interactions between environmental factors and a complex genetic background.1
At the cellular level, psoriatic plaques are characterised by:1
The epidermis has been identified as a key player in the early pathogenic steps of psoriasis by contributing to the activation of the immune response as well as the recruitment of inflammatory and endothelial cells.1
Risk factors
Psoriasis is a multifactorial disease that is associated with both genetic and environmental triggers or risk factors.2 It is estimated that approximately 10% of people inherit one or more of the genes associated with psoriasis, but only a fraction of them (2–3%) will go on to develop the disease.3
Several environmental risk factors have been associated with psoriasis.2–4
The elimination of psoriasis risk factors is important for controlling the disease.4
Underlying pathophysiology
The understanding of the pathogenesis of psoriasis has evolved significantly over several decades.5

Figure 1: Evolution of psoriasis pathophysiology5,8
The role of cytokines: TNF and IL-17/23
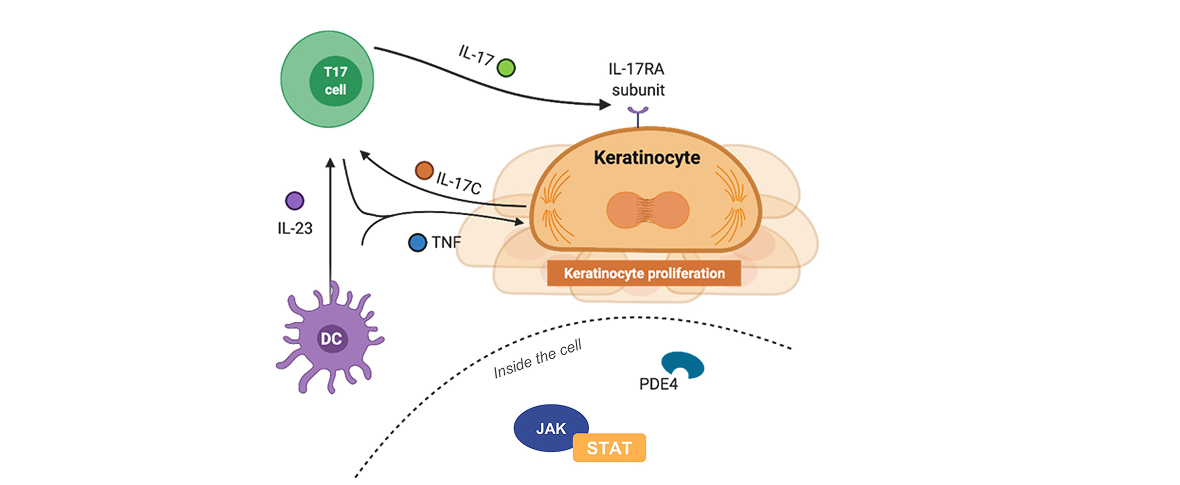
Psoriasis is thought to be a cytokine-led disease.5,6 Tumour necrosis factor (TNF) was one of the first cytokines to be defined as pathogenic in psoriasis. In synergy with TNF, the interleukin (IL)-17/23 axis is now known to also be central to psoriasis pathogenesis.7
The roles of IL-17 and IL-23 in the psoriasis inflammatory cascade have traditionally been illustrated by a waterfall hypothesis.
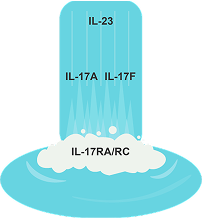
Figure 2: The IL-23/IL-17 axis waterfall hypothesis
However, we now understand that the processes involved in the pathophysiology of psoriasis are far more complex. Research into keratinocyte-produced factors shows that a feedback amplification loop drives the IL-17/23 axis and further amplification arises from the production of chemokines, which recruit immune cells to the lesion.8–11
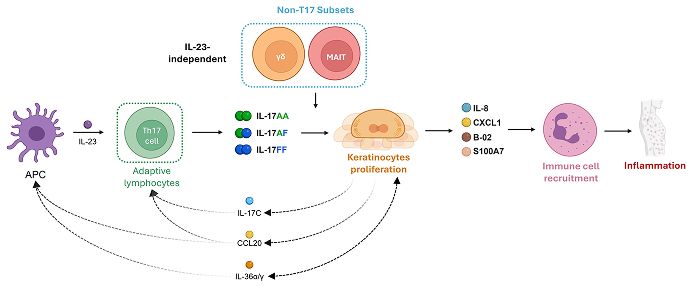
Figure 3: Psoriasis pathophysiology involves an amplification cycle that contributes to the development and maintenance of chronic inflammation12–15
The role of intracellular signalling: JAK/STAT
The JAK-STAT (Janus kinase–signal transducer and activator of transcription) pathway plays a crucial role in the intracellular signalling of many cytokines. Cytokines bind to extracellular receptors, causing the JAK-STAT cascade to activate downstream effects (e.g., producing inflammatory cytokines).11

Figure 4: The role of the JAK-STAT pathway in psoriasis11
The role of PDE4
Phosphodiesterase 4 (PDE4) is involved in regulating the inflammatory response at the molecular level and plays a key role in chronic plaque psoriasis and other inflammatory conditions. Degradation of cyclic adenosine monophosphate (cAMP) to adenosine monophosphate (AMP) by PDE4 leads to the production of pro-inflammatory cytokines (TNF, IL-23).16
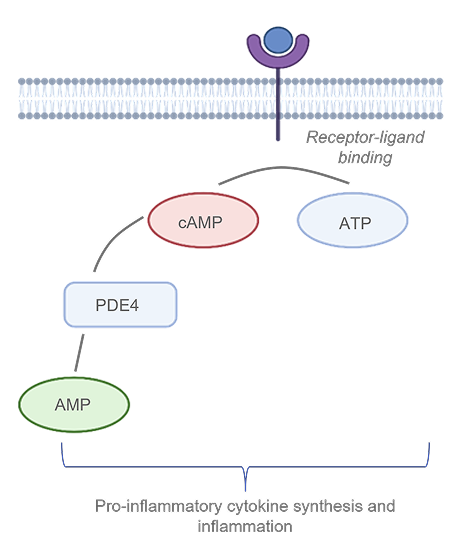
Figure 5: The role of PDE416
The importance of intercellular and intracellular mechanisms
Intercellular and intracellular mechanisms drive the pathogenesis of psoriasis together, and both can be targeted for treatment.5,6,8–11,16–19

Figure 6: Key mechanisms of psoriasis pathophysiology
Other articles you might like
You can read more articles that might interest you.
Want to see more articles?
Can’t find the answer you’re looking for? See all the Resources we have.