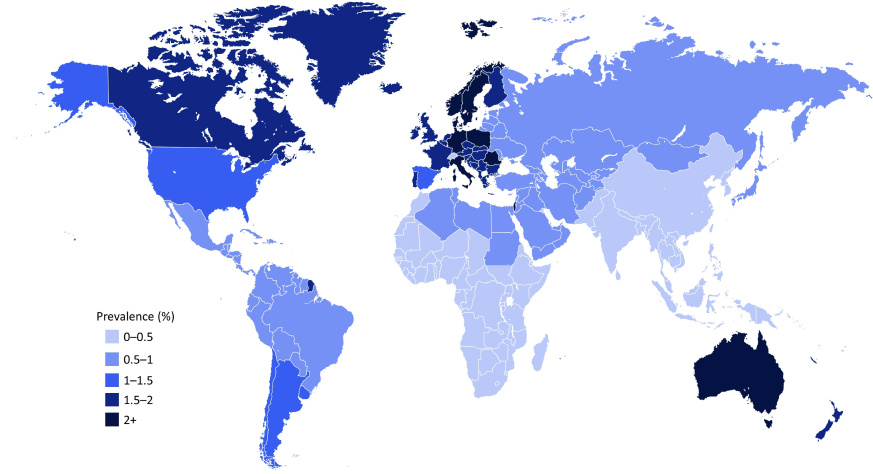
Figure 1: Heatmap showing the prevalence of psoriasis in both adults and children across the world8
The prevalence of psoriasis is steadily increasing over time.6,9 This may be due to increased awareness of the disease among physicians and patients.9
Who can be affected by psoriasis?
Women and men of all ages and ethnicities can be affected by psoriasis.10,11
The prevalence of psoriasis increases with age until approximately 60 or 70 years.9 Two peaks of psoriasis onset are observed at 30–39 and 60–69 years of age, which correspond with the classification of chronic plaque psoriasis as early-onset disease (type I; ≤40 years of age) and late-onset disease (type II; >40 years of age).9,12
Women and men are equally affected by psoriasis, although the age at psoriasis onset may be slightly earlier in women.9
The prevalence of psoriasis varies with ethnicity; White people are more likely to develop the condition than other ethnic groups.10,11
Symptoms of psoriasis
Symptoms of psoriasis can vary from person to person and generally include flaking, scaling, itching and scratching, rashes, skin pain, bleeding, redness, skin drying and cracking, and physical discomfort.11
Psoriasis can flare up anywhere on the body; symptoms mostly occur on the lower back, knees, elbows, legs, soles of the feet, scalp, face and palms, but can also affect the hands, nails, skin folds and genital area.2,3,11,13
Types of psoriasis3,12
There are many types of psoriasis, although plaque psoriasis is the most prevalent, comprising approximately 90% of all psoriasis cases.3,14